The Hidden Dangers of Parasitic Worm Infections
Parasitic worm infections also known as helminthic infections remain a major yet often underestimated global health concern. While many people associate these infections with remote tropical regions, they can occur in both developing and industrialized nations. Soil contamination, unsafe drinking water, undercooked food, international travel, and poor sanitation practices all contribute to transmission. The true danger lies not only in the immediate symptoms but in the long-term complications that can silently undermine health over months or even years.
Understanding the risks, mechanisms, and treatment strategiesv including sourcing medication from a reliable nizonide supplier is critical for effective management and prevention.
Types of Parasitic Worms That Infect Humans
Parasitic worms fall into three primary categories:
1. Roundworms (Nematodes)
Common examples include:
-
Ascariasis
-
Hookworm infection
-
Trichinellosis
Roundworms are typically transmitted through contaminated soil, food, or water. Some species can penetrate the skin directly.
2. Tapeworms (Cestodes)
These flat, segmented worms are usually contracted by consuming undercooked beef, pork, or fish. Species such as Taeniasis can live for years in the human intestine.
3. Flukes (Trematodes)
Flukes are often waterborne parasites. Schistosomiasis is a significant example affecting millions globally.
Each category presents unique pathological risks, but all share the potential for chronic health consequences if untreated.
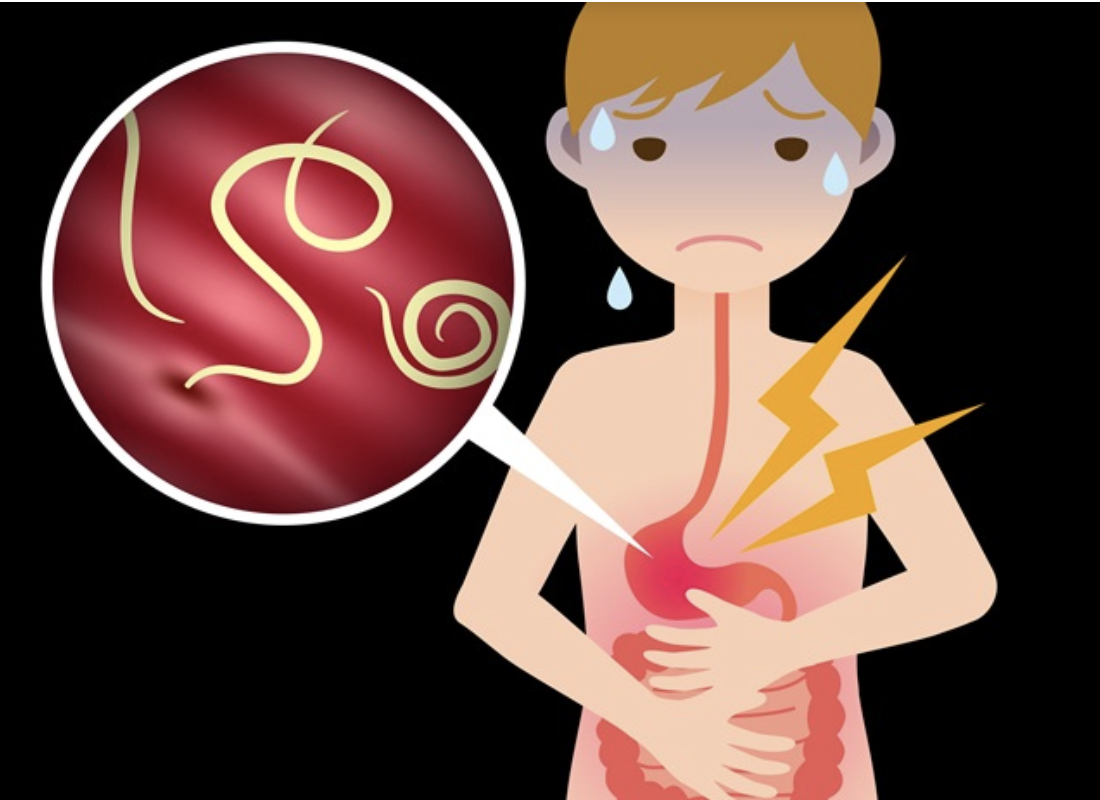
Subtle Early Symptoms That Often Go Ignored
One of the hidden dangers of parasitic worm infections is their nonspecific symptom profile. Early signs may resemble minor gastrointestinal disturbances, including:
-
Abdominal discomfort
-
Diarrhea or constipation
-
Nausea
-
Fatigue
-
Mild fever
-
Unexplained weight loss
Because these symptoms overlap with common digestive disorders, infections often go undiagnosed. In some cases, individuals remain asymptomatic for extended periods while internal damage progresses.
Nutritional Deficiencies and Malabsorption
Parasitic worms compete directly with the host for nutrients. Chronic infestations can result in:
-
Iron deficiency anemia
-
Protein-energy malnutrition
-
Vitamin deficiencies (especially B12 and fat-soluble vitamins)
-
Impaired growth in children
Hookworms attach to the intestinal lining and feed on blood, leading to significant iron loss. In endemic regions, this contributes to widespread anemia, particularly among pregnant women and children. Over time, untreated infections can compromise immune function and cognitive development.
Organ Damage and Systemic Complications
Beyond nutritional effects, certain worms migrate through tissues and organs, causing structural damage.
Liver and Biliary System
Flukes associated with Clonorchiasis can cause bile duct inflammation, fibrosis, and increased risk of malignancy.
Lungs
During larval migration, some roundworms pass through the lungs, triggering coughing, wheezing, and eosinophilic pneumonia-like symptoms.
Brain and Central Nervous System
Tapeworm larvae can invade the central nervous system, causing Neurocysticercosis. This condition may result in seizures, hydrocephalus, or chronic neurological impairment.
The delayed onset of these complications makes early detection essential.
Increased Vulnerability in High Risk Populations
Certain populations face heightened risk:
-
Children in areas with poor sanitation
-
Agricultural workers exposed to contaminated soil
-
Travelers to endemic regions
-
Immunocompromised individuals
In children, chronic helminth infections are associated with impaired cognitive performance and reduced school attendance. In pregnant women, anemia caused by worms increases maternal and fetal risks.
The Economic and Social Impact
Beyond physical health, parasitic infections contribute to a cycle of poverty. Chronic illness reduces productivity, increases healthcare costs, and places long-term strain on families and healthcare systems. In endemic areas, mass deworming programs are often implemented as a public health strategy to mitigate these effects.
However, treatment access and medication quality remain key determinants of successful outcomes.
Diagnosis and Laboratory Confirmation
Accurate diagnosis typically involves:
-
Stool microscopy for ova and parasites
-
Antigen detection assays
-
Serological testing
-
Imaging (for tissue-invasive species)
Because symptoms are nonspecific, laboratory confirmation is critical before initiating therapy. Misdiagnosis can lead to inappropriate treatment and persistent infection.
Treatment Options and the Importance of Reliable Medication Sources
Anthelmintic medications vary depending on the species involved. Common drug classes include:
-
Benzimidazoles (e.g., albendazole, mebendazole)
-
Praziquantel
-
Nitazoxanide
Nitazoxanide, often marketed under the brand name Nizonide, has broad-spectrum antiparasitic activity and is used for certain protozoal and helminth infections. When prescribing this medication, clinicians and healthcare distributors must ensure pharmaceutical-grade quality.
Working with a verified nizonide supplier is essential to guarantee product authenticity, regulatory compliance, and appropriate storage conditions. Substandard or counterfeit antiparasitic drugs can lead to treatment failure, drug resistance, and prolonged transmission cycles.
Pharmaceutical sourcing should prioritize
-
Good Manufacturing Practice (GMP) certification
-
Transparent supply chains
-
Batch traceability
-
Temperature-controlled logistics
For healthcare providers and distributors, selecting a reputable nizonide supplier directly impacts patient safety and therapeutic success.
Drug Resistance: A Growing Concern
Overuse or improper dosing of antiparasitic medications has led to emerging resistance patterns in certain regions. Incomplete treatment courses, poor-quality drugs, and lack of follow-up monitoring contribute to this problem.
Ensuring consistent dosing protocols and reliable pharmaceutical procurement reduces the risk of resistance development.
Prevention Strategies
Prevention remains the most cost-effective intervention. Key measures include:
-
Proper hand hygiene
-
Washing fruits and vegetables thoroughly
-
Cooking meat to safe internal temperatures
-
Wearing footwear in high-risk environments
-
Access to clean drinking water
-
Improved sanitation infrastructure
Public health campaigns emphasizing education and hygiene significantly reduce transmission rates.
When to Seek Medical Evaluation
Individuals should seek medical assessment if they experience
-
Persistent gastrointestinal symptoms
-
Unexplained anemia
-
Eosinophilia on blood tests
-
Seizures in endemic regions
-
Passage of worms in stool
Early diagnosis prevents complications and reduces transmission risk to others.
Conclusion
Parasitic worm infections represent a silent but substantial threat to global health. While early symptoms may appear mild or nonspecific, the long-term consequences including malnutrition, organ damage, neurological complications, and economic burden can be severe.
Effective management requires a multifaceted approach: accurate diagnosis, species-specific pharmacotherapy, prevention strategies, and access to high-quality medications. For healthcare providers and pharmaceutical distributors, partnering with a reputable nizonide supplier ensures the integrity of treatment regimens and safeguards patient outcomes.
Increased awareness, responsible medication sourcing, and proactive public health measures are essential to mitigating the hidden dangers of parasitic worm infections worldwide.
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Παιχνίδια
- Gardening
- Health
- Κεντρική Σελίδα
- Literature
- Music
- Networking
- άλλο
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness