IVF at Different Ages: What Really Changes
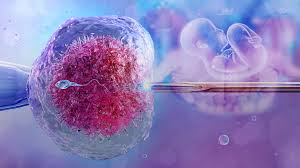
Age dominates fertility discussions, with "biological clock" warnings intensifying for women approaching their mid-30s. While this emphasis on age can feel judging and unfair, the biology is undeniable—age profoundly affects both natural fertility and IVF success rates. Understanding exactly what changes with age helps you make informed decisions about timing treatment and setting realistic expectations.
Female age at the time of egg retrieval is the single strongest predictor of IVF outcomes because it directly correlates with egg quality. While ovarian reserve (how many eggs remain) declines with age too, egg quality driven by chromosomal integrity matters more. Even one good-quality egg can result in successful pregnancy, while numerous poor-quality eggs yield no viable embryos.
IVF Success Rates Across Age Groups
IVF success rates decline steadily from women's early 20s through their 40s, with particularly notable drops after age 35 and again after 40. These statistics reflect population averages—individual women's outcomes vary based on numerous factors beyond age alone.
General live birth rates per IVF cycle:
- Under 30: 45-55% per cycle
- 30-34: 40-50% per cycle
- 35-37: 30-35% per cycle
- 38-40: 20-25% per cycle
- 41-42: 10-15% per cycle
- Over 43: 5-10% per cycle with own eggs
The dramatic decline after 37-38 reflects exponentially increasing chromosomal abnormality rates in eggs. At age 25, roughly 25% of eggs are chromosomally abnormal. By 35, this reaches approximately 50%. At 40, about 75% are abnormal. By 42, over 90% of eggs carry chromosomal errors incompatible with successful pregnancy even if fertilization and initial embryo development occur.
These statistics explain why even young women don't achieve 100% success—a quarter of their eggs are abnormal from the start. But the difference between 25% and 90% abnormality rates is enormous, dramatically affecting the likelihood that any given IVF cycle produces viable embryos capable of implantation and development.
Understanding these realities doesn't mean accepting defeat if you're over 35 or 40. Many women in these age groups succeed with IVF using their own eggs. The statistics simply inform realistic expectations about success probability and potential need for multiple cycles.
What Actually Changes in Your 30s
The transition through your 30s involves gradual changes rather than a sudden fertility cliff at 35. The "35 cutoff" represents a statistical inflection point where decline accelerates, not a biological switch that flips on your 35th birthday.
In your early 30s (30-34), fertility hasn't declined dramatically from your late 20s. IVF success rates remain quite good, typically 40-50% per cycle. Ovarian reserve generally remains adequate, allowing good response to stimulation medications. Egg quality, while slightly decreased from your 20s, still produces mostly chromosomally normal embryos.
Changes in early 30s:
- Slight decline in egg quality
- Minimal change in ovarian reserve for most women
- IVF success rates still quite favorable
- Less urgency than later 30s
- Generally good response to stimulation protocols
Mid-to-late 30s (35-39) marks more noticeable changes. Ovarian reserve declines become more apparent. AMH levels drop and antral follicle counts decrease, meaning fewer eggs typically retrieved during IVF cycles. More significantly, egg quality decreases noticeably, with chromosomal abnormality rates approaching or exceeding 50%.
IVF success rates drop to 20-35% per cycle depending on exactly where you fall in this age range. Protocol adjustments become more common—higher medication doses to recruit adequate follicle numbers, addition of supplements like DHEA or CoQ10 to potentially improve egg quality, and strong recommendations for genetic testing of embryos to identify chromosomally normal ones before transfer.
The Reality After 40
Fertility at 40+ faces significant challenges that can't be ignored or optimized away through lifestyle improvements. While some women over 40 successfully conceive with their own eggs through IVF, the statistics are sobering and should inform realistic decision-making about pursuing own-egg cycles versus considering alternatives.
At 40-42, IVF success rates with own eggs drop to 10-15% per cycle. Ovarian reserve has typically declined substantially, meaning you'll likely produce fewer eggs even with maximal stimulation. More critically, the vast majority of eggs—approximately 75-80%—are chromosomally abnormal, drastically reducing the probability that any given cycle yields viable embryos.
Challenges after age 40:
- Dramatically reduced egg quality
- Significantly diminished ovarian reserve
- Lower response to stimulation medications
- High probability no embryos reach transfer stage
- Increased cycle cancellation rates
- Need for multiple cycles to achieve success
After 43, success rates with own eggs drop to 5-10% per cycle or lower. At this age, over 90% of eggs are chromosomally abnormal. Many cycles produce no normal embryos suitable for transfer. Even when transfers occur, implantation rates are low and miscarriage risk is high due to the chromosomal abnormalities affecting most embryos.
These statistics aren't meant to discourage women over 40 from trying IVF if that's what they choose. However, understanding realistic probabilities helps with informed decision-making about how many cycles to attempt with own eggs before considering donor eggs, which offer dramatically better success rates regardless of recipient age.
How Protocols Change With Age
Fertility specialists adjust IVF protocols significantly based on age and ovarian reserve. Younger patients with good reserve might use relatively gentle stimulation to avoid overstimulation risk. Older patients typically receive more aggressive protocols maximizing egg numbers since each egg has lower probability of being chromosomally normal.
Medication dosages escalate with age and diminishing reserve. Where a 28-year-old might start stimulation with 150-200 IU of FSH daily, a 40-year-old might begin at 300-450 IU or higher. The goal shifts from preventing too many eggs to trying to retrieve adequate numbers given that most won't be usable.
Age-related protocol modifications:
- Higher starting medication doses
- Addition of growth hormone or DHEA supplements
- Longer stimulation periods if needed
- More frequent monitoring
- Strong recommendation for genetic testing
- Consideration of multiple retrievals to bank embryos
Genetic testing of embryos (PGT-A) becomes strongly recommended after 35 and almost essential after 40. Since chromosomal abnormalities are so prevalent, testing prevents transferring embryos destined to fail or miscarry. While PGT-A adds $3,000-5,000 to cycle costs, it improves per-transfer success rates by identifying the rare normal embryos among many abnormal ones.
Some doctors recommend "embryo banking" strategies for older patients—doing multiple egg retrievals to accumulate embryos before any transfers. This approach maximizes the number of embryos available for genetic testing, improving odds that at least some test normal. While costly and time-consuming upfront, banking potentially improves overall efficiency versus doing retrieval-transfer-failure cycles repeatedly.
The Emotional Experience Differs By Age
The psychological experience of IVF varies significantly depending on your age when pursuing treatment. Women in their 20s and early 30s, while distressed by needing fertility assistance, generally feel less time pressure than women approaching or past 40.
Younger patients might view a failed cycle as disappointment but know they have time for additional attempts. Older patients experience each failure more acutely—every cycle that doesn't work means several more months of aging, moving further into worse statistical categories with each passing month.
Age-related emotional challenges:
- Increased time pressure for older patients
- Regret about not trying earlier
- Fear of running out of time entirely
- Difficult decisions about when to stop trying with own eggs
- Grief about potentially needing donor eggs
Regret particularly affects women over 35, many of whom question whether waiting to try for children was a mistake. This regret persists even though career building, financial stability, or relationship timing that delayed childbearing were legitimate priorities at the time. Second-guessing past choices adds emotional weight to already difficult present circumstances.
Younger patients struggle with different challenges—feeling like fertility failure is unfair at their age, isolation from peers who conceive easily, and uncertainty about how long to pursue treatment before their fertility naturally declines. Both age groups face valid emotional struggles, just different ones based on their life stages.
Financial Implications Across Ages
Age affects fertility treatment costs in several ways. Older patients typically require higher medication doses, increasing pharmaceutical expenses. They're also more likely to need multiple cycles to achieve success, multiplying all costs.
Genetic testing becomes almost essential for older patients but adds $3,000-5,000 per cycle. Banking embryos through multiple retrievals before transferring means paying for multiple retrieval cycles upfront rather than doing one retrieval at a time. These financial realities mean pursuing IVF after 40 often costs significantly more than treatment at 32, even when cycle base fees are identical.
Age-related cost considerations:
- Higher medication costs with increased doses
- Multiple cycles more likely needed
- Genetic testing strongly recommended
- Potential embryo banking strategies
- Earlier consideration of donor eggs if own eggs repeatedly fail
On the other hand, women in their early 30s often face tighter financial constraints than those in their 40s who've had more years to build savings and advance careers. Balancing biological urgency against financial reality creates difficult trade-offs regardless of age.
For many couples, exploring treatment options at different locations helps manage costs. Seeking care where IVF center in Jaipur or similar quality clinics in smaller cities charge 30-40% less than premium urban centers allows more cycles within the same budget—particularly important for older patients likely needing multiple attempts.
When to Consider Donor Eggs
Donor eggs from young women (typically under 30) offer success rates of 60-70% per cycle regardless of recipient age. This dramatic improvement over own-egg success rates for older women makes donor eggs worth serious consideration after multiple failed own-egg cycles or when initial testing suggests very poor prognosis with own eggs.
The decision to use donor eggs is deeply personal and emotionally complex. Many women need months or years to process grief about genetic motherhood before opening to donor conception. This grief is legitimate and deserves adequate time and possibly therapeutic support to work through.
Considerations about donor eggs:
- Dramatically higher success rates than own eggs after 40
- Ability to experience pregnancy and birth
- Genetic connection to partner (if using partner sperm)
- Emotional processing of non-genetic motherhood
- Costs typically higher than own-egg IVF
- Legal considerations depending on location
Some women know relatively quickly that donor eggs feel acceptable to them—they prioritize experiencing pregnancy and becoming parents over genetic connection. Others never feel comfortable with donor conception and pursue adoption, surrogacy, or child-free living instead. Neither response is right or wrong; they simply reflect different personal values and priorities.
Clinics typically suggest considering donor eggs after 3-4 failed own-egg IVF cycles, though this varies based on age and specific circumstances. A 44-year-old might discuss donors after one or two failures given very low success odds with own eggs. A 38-year-old might reasonably try more own-egg cycles before switching approaches.
Advice for Different Age Groups
If you're under 30: You likely have time before fertility urgency becomes critical, but don't assume you have infinite time. If you've been trying to conceive for a year without success (or six months if you have known risk factors like PCOS or endometriosis), consult a fertility specialist. Sometimes simple interventions solve the problem without IVF. Don't wait years assuming you're "too young" to have fertility problems.
If you're 30-34: You're in a good position age-wise for IVF success if needed, but don't procrastinate if you know you need treatment. Each year you wait, success rates decline and costs potentially increase. If testing reveals issues best addressed with IVF, starting sooner rather than later makes sense even if you feel you "have time."
If you're 35-39: Time urgency increases substantially. Don't spend years on low-probability interventions like timed intercourse with oral medications. If IVF is indicated, pursue it without delay. Consider being more aggressive with protocols and interventions like genetic testing. Every few months matter at this age—don't let fear or procrastination waste precious time.
If you're 40+: Be realistic about own-egg success probability while also knowing success is possible. Set limits before starting—you'll try 2-3 own-egg cycles, for example, then move to donor eggs if unsuccessful. Don't spend years and tens of thousands of dollars pursuing own-egg cycles with very low success probability when donor eggs offer much better odds.
The Bottom Line on Age and IVF
Age profoundly affects IVF success rates through its impact on egg quality and quantity. These effects are biological realities, not judgments about when you "should have" tried for children. Understanding age-related fertility decline helps you make informed decisions about treatment timing and setting realistic expectations.
However, age doesn't determine your worth, and fertility struggles aren't your fault regardless of when they occur. Women at every age deserve compassionate, expert care as they pursue family building. Whether you're 28 or 42, your desire for children is valid and your fertility treatment journey deserves support.
If you're considering IVF, don't let age fears paralyze you into inaction. Consult with fertility specialists about your specific situation—your ovarian reserve, diagnosis, and individual circumstances matter as much as your age. Make decisions based on complete information rather than assumptions, and remember that statistics describe populations, not individuals. Your outcome will be your outcome, influenced by but not determined solely by your age.
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- الألعاب
- Gardening
- Health
- الرئيسية
- Literature
- Music
- Networking
- أخرى
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness